Published on December 7, 2017
An unconscious patient rolls into an ER with no ID except for a “Do Not Resuscitate” tattoo across his chest. Should doctors save his life, or is the DNR tattoo legally binding?
Estate planning attorneys Foster Friedman and Gretchyn Meinken say this fascinating New York Times article reminds us there are better ways to declare your medical decisions. Are your Advance Medical Directives up to date? For any questions contact Foster or Gretchyn.
Virginia residents can store their documents in the Virginia Advance Health Care Directives Registry for emergency responders and family members to access.
As seen on The New York Times:
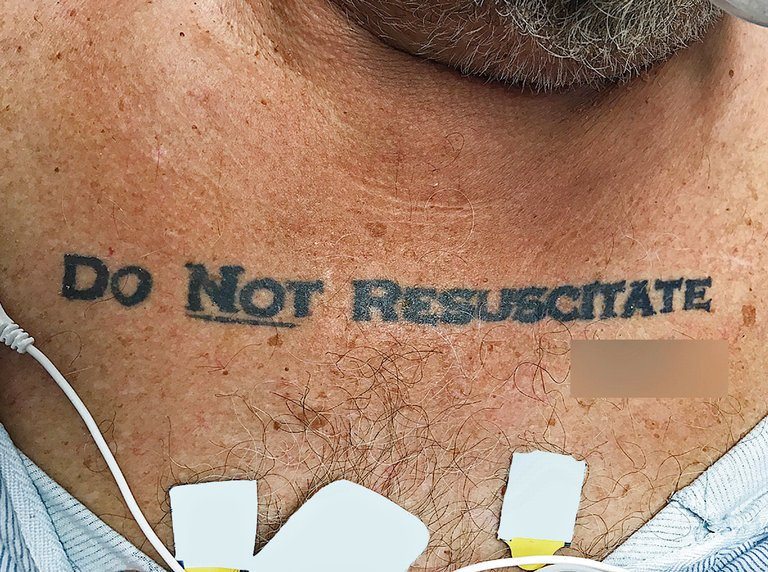
A man in Miami took extra care to make sure his end-of-life medical treatment went according to his wishes: He had the words “do not resuscitate” tattooed on his chest.
The black, bold capital letters were in plain sight on his collarbone. The word “not” was underlined, for good measure. And the man’s own signature was reproduced beneath the demand.
It worked, in a way. The man, 70, had a history of lung disease, heart problems and diabetes when he was admitted to the Jackson Memorial Hospital this year. He was unconscious and did not have any identification. His blood alcohol level was high.
According to a letter published in The New England Journal of Medicine on Thursday, doctors administered some treatment, but the man never became responsive enough to speak. And while the message of the tattoo was clear, doctors had no way of knowing whether getting it had been an impulsive decision.
So they consulted an ethics expert, Kenneth W. Goodman, who advised them to honor the man’s apparent wishes. The doctors stopped short of administering the most invasive forms of lifesaving treatment, and the man’s health deteriorated until he died.
Dr. Goodman, the director of the Institute for Bioethics and Health Policy at the University of Miami’s Miller School of Medicine, decided at the time that the tattoo seemed very deliberate.
“Here’s a guy who went through the trouble of getting a tattoo, which has the word ‘not’ underscored; he had his tattoo artist include his signature,” Dr. Goodman said in a phone interview on Sunday. “You don’t go through that trouble, look at it every day in the mirror and actually not mean it.”
Nancy Berlinger, a health care ethics expert and research scholar at the Hastings Center, said the doctors did well to consult an expert and honor the patient’s wishes.
She added that there is a growing movement to improve the way doctors and patients communicate about end-of-life care, but there is still a long way to go. Many people are reluctant to discuss mortality, even with close friends and family. Some patients may not trust health care facilities to keep track of their preferences. And standards for notifying doctors about end-of-life care or resuscitation wishes can vary across state lines, or even from one hospital to the next.
“There’s this impasse that we haven’t figured out how to cross,” Dr. Berlinger said. “And this man was trying.”
In the United States, people have the right to ask not to be resuscitated in the event of a medical emergency, and they can make their wishes known ahead of time in case they one day find themselves incapacitated and alone. Different states have different ways of documenting these wishes (though none involve tattooed clavicles). In Florida, a patient can fill out a particular form.
Before the man in Miami died, the doctors discovered that he had indeed filled out the form in advance. He did not have it on him when he arrived at the hospital, but social workers found it after he was admitted.
Ultimately, the tattoo “produced more confusion than clarity,” the doctors said in the letter. “This case report neither supports nor opposes the use of tattoos to express end-of-life wishes when the person is incapacitated.”
Dr. Goodman said the case could heighten public awareness of advance directives — documents that outline wishes for end-of-life care ahead of time — because people tend to think more about their futures when dramatic stories like these make headlines.
“Attention to the importance of advance directives is episodic,” he said. “If you’re an adult, you really should talk to family members and friends about what you would want.”